What Does Housing Have To Do With Healthcare?
In short, housing is healthcare. Over 1,000 people registered for this year’s Health Care for the Homeless Conference in Baltimore, May 15th – May 19th. I attended various sessions that focused on the ties between health and housing, as well as the benefits of recuperative care for our neighbors experiencing homelessness. The presentations were substantive. I was a first-time attendee and went in with an open mind, hoping to come away with gained knowledge and a narrative succinctly describing the undeniable connections between improved health markers and safe and stable housing.
There was much discussion about the social determinants of health vs. the structural determinants of health. In Houston, for example, Ben King, Ph.D. M.P.H. of the University of Houston said the life expectancy of an unhoused woman in Houston is 47 years and that, in the US, one unsheltered person is dying on the streets every three days. Homelessness cuts a person's lifespan nearly in half. Half. Let that sink in for a moment. Poverty is much harder to recover from than mental health because housing can be fluid; from tent to housing to tent and so on. In addition to the housing loop, a crisis cycle shortens lifespans and strains public services.
Health Care for the Homeless [annual] Conference and Policy Symposium’s theme for 2023 was Toward Justice: Leading with Lived Expertise.
Breaking the Cycle
One of the presentations I attended showed the flexible housing pool in Chicago and Cook County. Through data, the Center for Housing and Health and Cook County Health identified whom to target for housing and supportive services. They could see who was cycling through the crisis systems of emergency rooms to jails to shelters and had chronic health issues because of being stuck in this loop. Cost reduction for these services translates into cost savings for institutions and taxpayers alike. Throughout the conference, I heard cost estimates for hospitalizing an individual without insurance ranging from $3,000-$6,000 per night. This team’s goal was to use the data captured by hospitals, jails and shelters to connect those individuals with the appropriate services and housing to break the non-stop need for public services.
Aging in Place
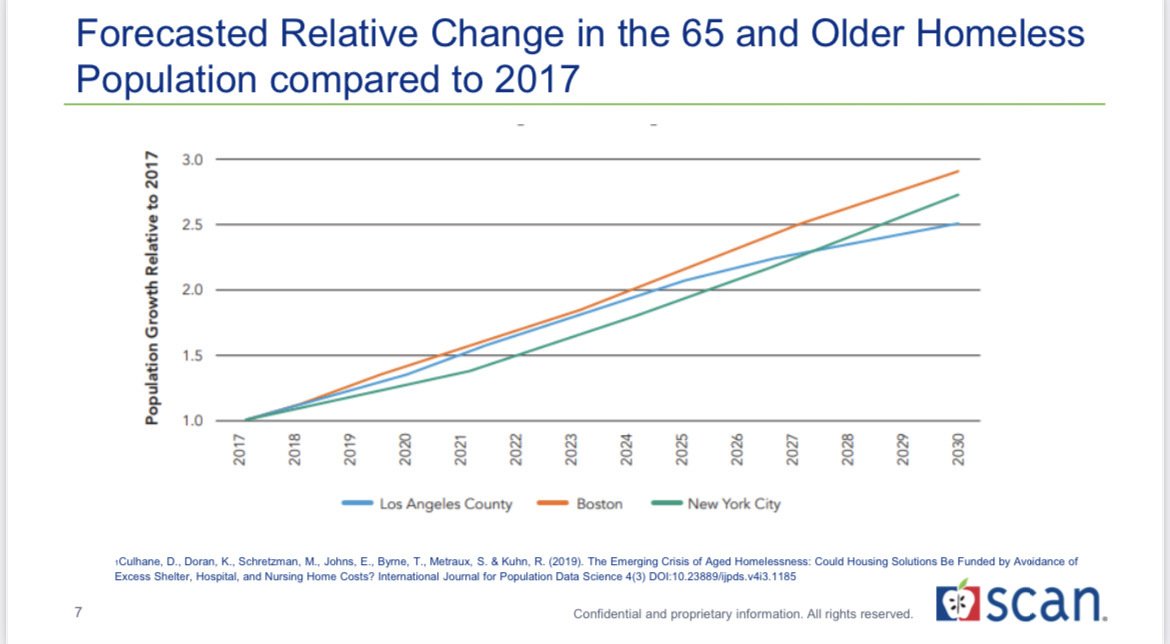
SCAN HealthPlan, an organization from LA, serves seniors at risk of or currently experiencing homelessness through a three-pronged approach: Housing and Healthcare Member Benefits, Housing Services to the community at large and medical street outreach. They discussed the “silver tsunami” of seniors in the baby boomer generation that will undoubtedly overwhelm the healthcare system that is already short-staffed. Seniors are one of the most at-risk groups in our country for losing housing and essential care due to a lack of resources and financial income.
‘Housing the Impossibles’ presentation discussed how to house the medically frail homeless population. When a person is not physically able to dust and clean, these tasks are impossible without outside help, and since their goal is to empower seniors to age in place, they engaged volunteers to help aging residents with limited abilities keep their rooms tidy. People are often kicked out of housing if they are unable to keep their living space neat and clean, so these volunteers are lifesavers. Additionally, Cardea Health put together an ethics panel of attorneys, staff and community stakeholders to help staff and volunteers navigate secondary trauma and devise a plan for their clients who refuse help.
Naming Your Needs
A common topic discussed at the conference was the importance of meeting individuals where they are by implementing measures like harm reduction and home health visits to break down the barriers of fear and trauma tied to hospitals and medical care. The various speakers and frontline workers in attendance stressed the importance of engaging people with lived expertise to ensure outcomes reflect the true needs of clients. People are complex; therefore, homelessness is a complicated issue that requires empathy to achieve successful outcomes.
Marisa, the Homeless Outreach Team Coordinator at Opportunity Council in Bellingham, Washington, took me under her wing, even taking notes for me at times. Like others in the crowd, she possessed the patience of a saint and the grit of someone hellbent on solving a seemingly impossible problem.
The general rules for the Housing First model are:
A client cannot use substances in their unit
Case management for substance abuse and mental health must be administered
And the rules are set by the service provider
Wet Housing on the other hand:
Allows clients to use substances in their units
Has relaxed rules in place
Is very tolerant and has a low eviction rate
Wrap-Around or Supportive Services are based on collaborative care with the SMART Philosophy:
Short
Measurable
Achievable
Reachable/Realistic
Time-Bound
In closing, I am inspired by the work happening on the front lines and HomeAid affiliates will continue innovating and employing the perspectives of people with lived expertise to support those frontline efforts and build a future without homelessness. There is immense value in creating spaces that are client-driven and effectively serve their unique needs. Housing and healthcare are human rights that work independently and in tandem with one another, contributing to the quality and quantity of life, and when community stakeholders collaborate to make housing attainable, everyone wins.